COVID-19 variants continue to emerge and diverge from the initial strain first identified in the winter of 2019. Today, the most prevalent strain is the Delta variant, but new cases involving the Omicron variant are sparking concern.
The initial strain of SARS-CoV-2 rapidly spread around the world and was constantly surveilled by multiple health organizations.
The Center for Disease and Control (CDC) monitors SARS-CoV-2 variants, which can be classified into four categories. Variants Being Monitored (VBM) are variants that do not have a significant public health risk. Variants of Interest (VOI) have mutations that may lead to less efficacy of treatments and a higher attack rate. Variants of Concern (VOC) cause an increase in severity of the disease and are more transmissible, including among vaccinated populations. Variants of High Consequence (VOHC) mean that prevention measures, such as vaccines, do not work. Currently, there are no VOHC.
SARS-CoV-2 is an RNA virus; its genetic material is RNA, not DNA. The RNA Dependent RNA polymerase (RDRP) has lower fidelity than DNA polymerase, so it makes more mistakes than DNA viruses. RNA viruses generate mutations more quickly, which is evolutionarily advantageous to the virus but detrimental to humans.
The SARS-CoV-2 virus has a protein called a Spike, which allows itself to enter cells via binding to ACE2 receptors. It is also the most exposed part of the virus, so it is most likely to be attacked by antibodies from the body’s immune system that can neutralize the virus. However, the virus can create mutations on the Spike protein to evade antibodies and continue to spread.
Sometimes, new variants fizzle out.
Joe DeRisi, a professor at UCSF and the co-President of the Chan-Zuckerberg Biohub, runs a COVID testing site in the Mission and is one of the world’s leading experts on SARS-CoV-2. At this site, DeRisi and other scientists from UCSF track positive cases and their mutations.
“Every time we sequence positive samples from the Mission, there are always new mutations. Dozens of new mutations, all over the Spike protein. Most of which we see once, and only once, and we never see them again. And it’s because they have no clinical significance — they don’t do anything,” DeRisi said.
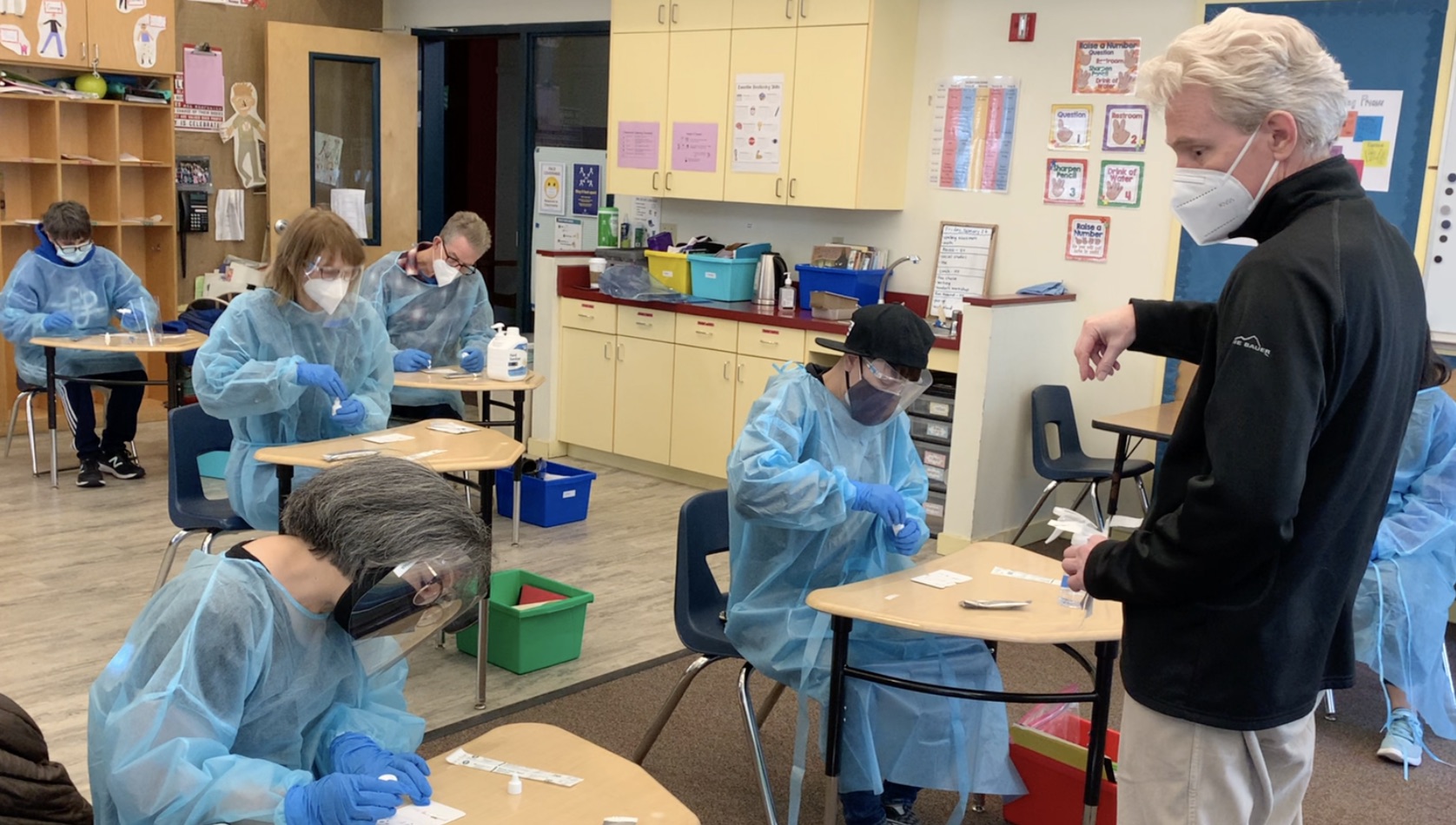
photo courtesy of Joe DeRisi
In other cases, such as the Delta and Omicron variants, these new variants become more prevalent and are often more transmissible and dangerous.
With Omicron, “seeing a bunch of mutations all at once and seeing them in more than one patient makes people pay attention,” said DeRisi.
The Delta variant is currently the most common strain in the United States. It is a VOC, as it has several Spike protein mutations that cause it to have increased transmissibility — possibly twice as much as other variants according to the CDC — and viral load in comparison to the initial strain from Wuhan.
In order to determine if a person infected with COVID is afflicted with a variant, they can receive testing and their samples can be sequenced. Testing can be done through polymerase chain reaction (PCR) testing, which converts the RNA of the virus to DNA and amplifies it to detect COVID-19 using specific primers. Antigen testing uses a technology called a lateral flow assay to detect the nucleocapsid (N) protein using antibodies.
The positive COVID cases are sequenced by gathering the RNA from the virus, converting it to DNA and running it through sequencing on the Illumina platform that generates the sequence data. Scientists then compare the sequence to the original SARS-CoV-2 strain to see mutations. These mutations are uploaded to an international database to track the epidemiology of the variants in the form of phylogenetic trees.
While PCR samples are commonly used to sequence COVID samples, DeRisi discovered how to also sequence samples collected from antigen tests. This allows testing sites that use antigen tests — which are far more accessible and rapid than PCR — to send samples to labs. Thus, there is a diverse collection of data that paints an accurate map of the spread of COVID from community-based testing sites.
A successful measure against COVID-19 is getting vaccinated. But as new mutations continue to arise, the vaccine loses its efficacy.
Vaccines were developed for the initial strain of COVID-19. This means that they generate neutralizing antibodies against the Spike protein of the virus from Wuhan. They are less effective against variants like Delta since the Spike protein has changed and the neutralizing antibodies cannot bind to the Spike protein as well. There is concern if a variant is mutated enough such that it renders the vaccine completely ineffective.
The Delta variant has 13 mutations on its Spike protein, meaning that 13 of the amino acids it produces differ from the initial strain of COVID-19. Though vaccines work well on reducing the infection of the Delta variant, if future variants have more Spike protein mutations, the vaccine can further lose its effectiveness.
Adults who have been vaccinated for over six months are eligible to receive booster shots. However, the boosters have not been adapted to fight mutations of COVID-19.
On November 25, South Africa’s health minister announced a new variant, dubbed the Omicron variant. It is classified as a VOC.
However, data on the Omicron variant is still limited.
“There are fewer than 120 sequences that have been documented so far, so it’s a tiny number. It has a lot of changes to Spike that are very unusual. Unlike the Delta variant, it has several mutations that are not usually seen, and the significance of these mutations is really unknown,” said DeRisi.
Scientists have discovered that this variant has 32 mutations on its Spike protein, which is more mutations than any other variant. It is unusual for a variant to jump to 32 mutations. However, Africa has a very low vaccination rate compared to the rest of the world, and though low positive cases have been reported from the continent, this is likely due to a lack of testing resources. Few samples are being detected or sequenced by labs, and so lots of evolution could be taking place under the radar.
“Right now, we don’t know if the Omicron variant is more infective, less infective, more transmissible or less transmissible. We don’t know about disease severity. We don’t know about vaccine resilience. Until experiments can be done in the lab, we really can only go on the numbers from epidemiology, which right now, are too small to say anything significant,” DeRisi said.
DeRisi’s lab currently does not have access to sequences of the Omicron variant, as there is no centralized repository for RNA viruses. They cannot easily create pseudoviruses — safe versions of SARS-CoV-2 with only the mutated Spike protein — to test the significance of variants and if they can be neutralized with the vaccine, unless they have that material.
There is also a lack of information on the severity of the Omicron variant because there are not enough hospital case reports to have this information.
While scientists wait for new information, Moderna announced that the company is working on vaccines against the Omicron variant, either through an increased dose of the current vaccine or through the development of a vaccine with neutralizing antibodies targeted at the Spike protein of new variants. Pfizer claimed that it can create a vaccine against the Omicron variant in the next 100 days, and Johnson & Johnson is beginning to test their Omicron-specific vaccine. But so far, no company offers vaccines against specific COVID variants to the public.
In response to news about the Omicron variant, several countries, including the U.S., decided to ban travel to and from South Africa. Still, cases have spread outside the region.
Strict travel restrictions — such as Australia’s rule of spending two weeks in a hotel after traveling — can help prevent the spread of COVID-19. However, the U.S. has struggled with effective travel limitations thus far into the pandemic.
The first case of the Omicron variant in the U.S. was announced on December 1. An individual had traveled to San Francisco from South Africa on November 22. Several other cases of the Omicron variant in the U.S. have been detected as well.
The Chief Medical Advisor to the President, Dr. Anthony Fauci, said to reporters, “We knew that it was just a matter of time before the first case of Omicron would be detected in the United States.”
He stressed the importance of vaccines and booster shots to provide protection while scientists research the severity of the Omicron variant.
During the cold winter months and holiday travel season last year, the U.S. and much of the global population saw an uptick in COVID-19 diagnoses. Experts predict another increase in cases this year, with the Omicron variant adding additional concerns.
Public health officials advise people to adopt a Swiss Cheese Model of defense against COVID-19, meaning people should wear masks, get vaccines, have regular testing and social distance when possible. While certain protections may become less effective as the virus mutates, the best way to prevent the spread of COVID-19 is to practice multiple defenses — none of them is perfect, but together they work to reduce the risk of catching COVID-19.





